How a scientist interprets outcomes often depends on whether she thinks the outcome should be good or bad.
Cortisol levels make a good example.
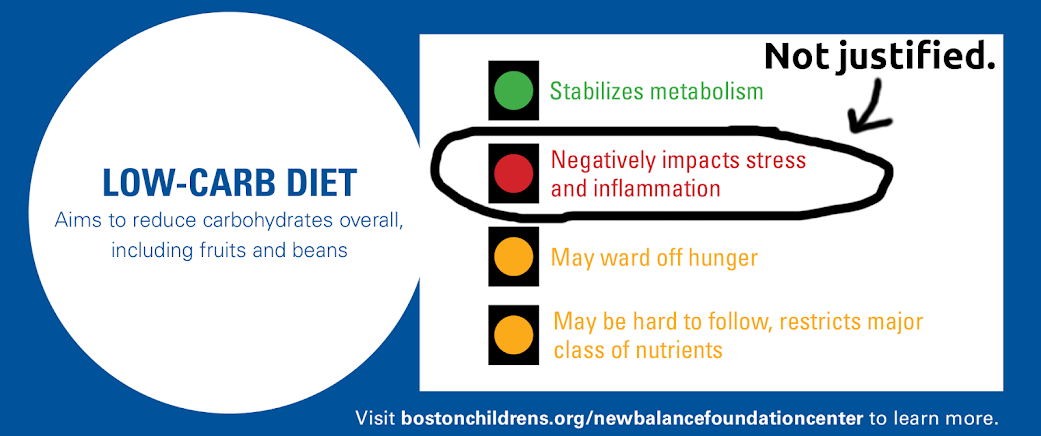
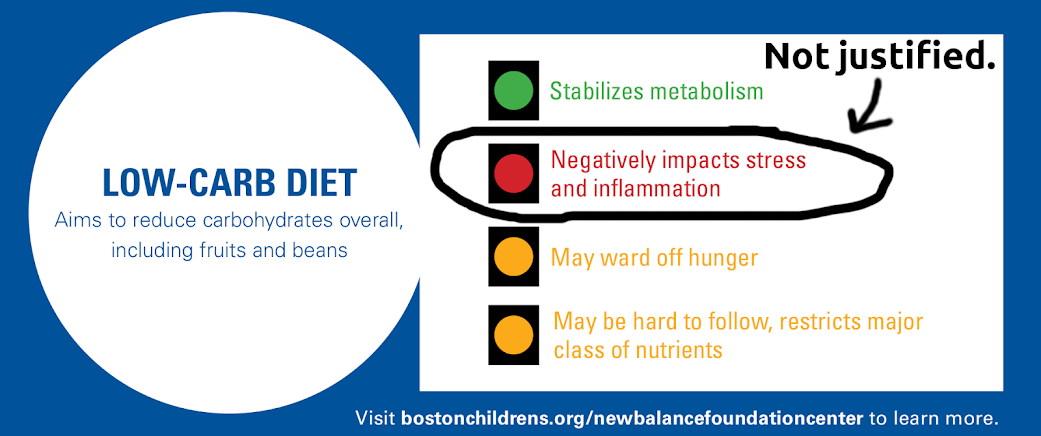
In the context of low carb, ketogenic diets, the finding of slightly higher cortisol levels have been interpreted as a warning sign. In a recent post on our blog, Zooko and I attempt to explain why the “red light” that Boston Children’s Hospital gave low carb diets is not justified.
It is interesting to note that while cortisol sends up red flags for ketogenic diets, which mainstream medicine actively disapproves of, it sends up green flags in another context: longevity research.
Time and again I have come across glib statements in longevity papers saying that the beneficial, health-enhancing and lifespan-increasing effects of caloric restriction probably come in part from the moderately increased cortisol that is consistently seen in calorie restricted animals. The intuitiveness of the beneficial effects of cortisol is usually based on cortisol’s known anti-inflammatory action.
Here are just a few such quotes:
- “The mechanisms responsible for calorie restriction–mediated beneficial effects on primary aging observed in rodents probably involve the metabolic adaptations to restriction itself, including… a modest increase in levels of circulating cortisol, which result in a reduction in systemic inflammation.”
— Aging, adiposity, and calorie restriction. Fontana L, Klein S. JAMA. 2007 Mar 7;297(9):986-94. - “Even short-term DR can attenuate inflammation and affect metabolic and DNA repair pathways. Mechanisms by which DR suppresses peripheral inflammation include the elevation of glucocorticoids, lowering of glucose and activation of PPARs. Although the effects of DR are less understood in the brain, common pathways are emerging that link many normal aging inflammatory processes with age related diseases such as AD, cancer, diabetes and cardiovascular disease.”
— Anti-inflammatory mechanisms of dietary restriction in slowing aging processes. Morgan TE, Wong AM, Finch CE. Interdiscip Top Gerontol. 2007;35:83-97. - “Glucocorticoids are yet another class of hormones that may contribute to the anticarcinogenic action of DR [101, 102]. Total and/or free glucocorticoid levels are increased by DR [103–105]. Glucocorticoids suppress cellular proliferation and enhance apoptosis in a number of cell types, including osteoblasts, lymphocytes and keratinocytes (for reviews, see Weinstein [106], Herold et al. [107] and Budunova et al. [108]). In humans, glucocorticoids are effectively used for treating lymphoid neoplasms [109]. Importantly, adrenalectomy abolishes the protective effect of DR on skin and pulmonary carcinogenesis, while glucocorticoid replacement restores this protection [110–112].
— Can short-term dietary restriction and fasting have a long-term anticarcinogenic effect? Klebanov S. Interdiscip Top Gerontol. 2007;35:176-92. - Another mechanism by which CR may selectively exert it’s anti-inflammatory effects is via enhanced endogenous corticosteroid production (Sabatino et al. 1991). Chronic CR potentiates the diurnal elevation of plasma corticosterone. CR mice and rats have “moderately” but significantly higher daily mean plasma free corticosterone concentration than mice fed “ad libitum” throughout their lifespan…
It is well known that the hypothalamic–pituitary–adrenal axis and glucocorticoids in particular are essential in limiting and resolving the inflammatory process (Sapolsky et al. 2000). Glucocorticoids have pleiotropic inhibitory effects on the immune system and inflammatory gene expression (Rhen and Cidlowski 2005). In addition, treatment with pharmacological doses of exogenous glucocorticoids has been used to block many inflammatory and autoimmune diseases, including rheumatoid arthritis, systemic lupus erythematosus, Graves’ disease, thyroiditis, glomerulonephritis, multiple sclerosis, and psoriasis.”
— Neuroendocrine Factors in the Regulation of Inflammation: Excessive Adiposity and Calorie Restriction Luigi Fontana, Exp Gerontol. 2009; 44(1-2): 41–45.
I particularly like that last one, because of the use of the word “enhanced”, which connotes that the thing that has increased is surely a Good Thing.
Now of course, the longevity researchers can’t pick up on a significant difference between the animals that lived longer and those that didn’t and say: Well, the diet might be good for some things, but this difference warrants caution.
They can’t do that because the end outcome is definitive.
It’s true that there is a significant school of thought that says that longevity is a result of hormesis. The hormetic explanation amounts to “what doesn’t kill you makes you stronger.” That way a researcher gets to say that phenomenon X is bad for you, and that things that are bad for you improve your health. It is a way out of a paradox, as expressed nicely here:
“One well-known, exemplified response to stress is the hormonal increase in adrenal corticosterone levels in plasma during aging, where increases in these levels appear to be proportional to the degree of stress. Aged animals appear to have a diminished ability to attenuate the increase, causing the aged to have continually elevated plasma levels of corticosterones. These authors suggested that increased levels of corticosterone in aged rats result in hippocampal neuronal cell death, that is, the stage of exhaustion. However, this scenario in the glucocorticoid cascade hypothesis is obviously not applicable in the case of the CR paradigm, because CR results in an increased life span in spite of chronically elevated diurnal levels of serum corticosterone. This apparent contradiction makes the interrelation of glucocorticoid and aging far more complex than one might want to narrowly define it and needs other mechanistic explanations like stress resistance to resolve the disparity in responses.” — Stress resistance by caloric restriction for longevity. Yu BP, Chung HY. Ann N Y Acad Sci. 2001 Apr;928:39-47. (my emphasis)
As Carol Loffelmann recently said on twitter: Scientists who discover paradoxes should examine their initial assumptions.
So supposing we have a study showing that a group that looks healthier than the other groups in essentially every measure also has higher levels of cortisol.
We can reason, as Ebbeling et al. do, that since higher cortisol is associated with bad health outcomes, the ketogenic diet may be dangerous, despite the other measures.
Or we can reason, as the longevity researchers do (and as Zooko and I did), that since the group is healthier, higher cortisol must be exerting or reflecting a healthy process, and this may present a paradox that we as researchers have to resolve.
Allow me one further point:
The findings of higher cortisol in calorie restricted animals is itself a body of literature of relevance here.
Anyone finding that their intervention moderately elevates cortisol can and should now say: Higher cortisol levels are found in animals whose lifespans have been increased experimentally by dietary intervention, and so this finding in our intervention could be indicative of a longevity-inducing effect.
My current micro-obsession is how to create a negative lipid balance – increase lipolysis and lipid oxidation. Turns out cortisol may be beneficial – "Increased cortisol secretion during prolonged fasting may partially account for this effect, as it is known to stimulate lipolysis at physiologically high levels (Djurhuus et al., 2002)" – from http://journals.humankinetics.com/AcuCustom/Sitename/Documents/DocumentItem/4945.pdf
Hi PhilT. Yes, another relevant point about cortisol is that its effects depend on insulin state. Higher cortisol in high insulin conditions leads to more fat storage, higher cortisol in low insulin conditions leads to more fat burning.
This seems exactly the point that proves it is not a paradox. Systemic insulin levels. My curiosity here includes whether or not increases in glucocorticoids themselves increase blood glucose during CR or fasting and provoke insulin spikes high enough to shutdown ketosis?
Suggestion. Cortisol is a metabolite of progesterone. Adequate progesterone in the body will act as the body's main anti-inflamatory if there is enough progesterone to do the job, without any of the bad side effects cortisol is known for. The problem is that most of us (men and women) are estrogen dominant and progesterone deficient. Enough progesterone will probably produce all of the advantages of cortisol you mention and with none of its downsides. I am 63 years old, was testosterone deficient, was put on testosterone and it jacked my estrogen levels so high I got gynocomastia. Topical, bioidentical progesterone (easily found online or in health stores) changed that literally overnight. So I kept using it and then discovered I didn't need testosterone supplements any more either and they had normalized without testosterone supplementation. For two years now I have taken 60 mg of progesterone a day, primarily for anti-inflamatory reasons. I had a laminectomy in 1998 that resulted in severe knotting of the muscles of my low back. Testosterone really reduced the size of these knots and then I discovered progesterone did the same thing.
By the way I have been an Atkins dieter since 1995, but have always found ketosis very difficult to maintain. I am now discovering it was probably due to too much protein intake since I have never had difficulty doing carb restriction. So I an now trying to see if getting off all grains entirely and cutting down on proteins will help get me into some sustainable level of ketosis. I am quite keto resistant, probably from all the years of carboyhdrate restrictions. My body must have keto adapted in the wrong sense. I must be great at turning proteins into sugars.
How are you faring now?